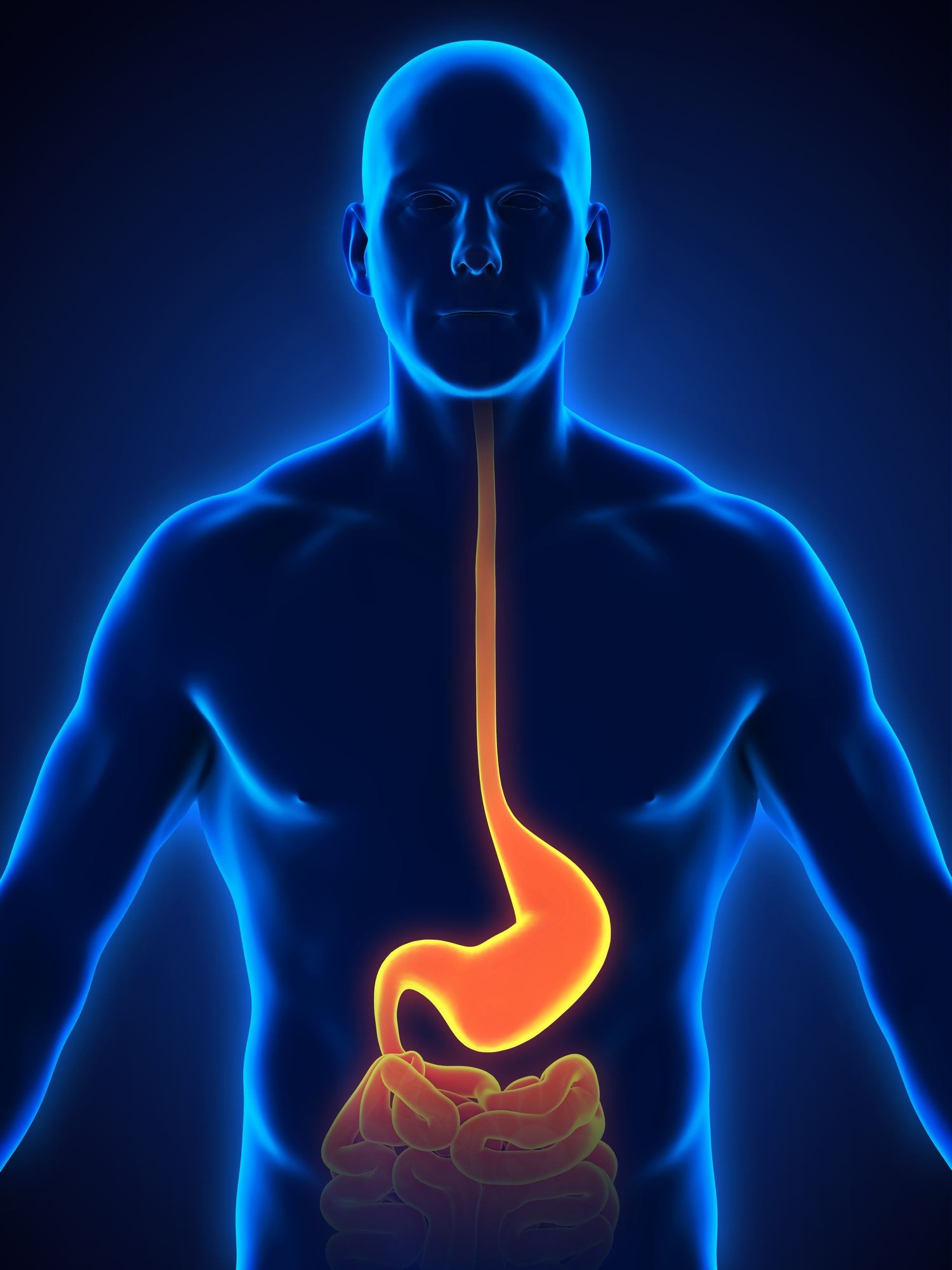
People who suffer from gastroesophageal reflux disease (GERD) can sometimes develop a potentially dangerous condition called Barrett’s esophagus.
Barrett’s esophagus causes the cells lining the esophagus to change into cells similar to those in the intestine. It’s the body’s reaction to long-term exposure to stomach acid that flows back, or refluxes, into the esophagus from GERD.
Barrett’s and GERD
An estimated 20 percent of Americans have GERD, which occurs when the muscle that acts as a valve between your esophagus and stomach doesn’t work correctly allowing acid to flow back up into the esophagus.
Common GERD symptoms include:
- A burning sensation in the chest or throat (heartburn), sometimes with a sour taste in your mouth
- Trouble swallowing or a chronic sore throat
- A feeling of a lump in your throat
- Dry cough
There are no specific symptoms associated with Barrett’s esophagus, and it’s usually detected during an endoscopy to diagnose GERD. However, GERD doesn’t always cause symptoms. Endoscopy screening for Barrett’s may be recommended for certain patients who don’t have any symptoms, including those with a family history of esophageal cancer.
Fortunately, only a small percentage of people with GERD develop Barrett’s esophagus. The average age of diagnosis is 50, and it is more commonly seen in men; particularly Caucasian men. Once a person is discovered to have Barrett’s esophagus, regular endoscopy screening is required to check for dysplasia, a precancerous condition in the esophagus. Dysplasia puts you at high risk for developing esophageal cancer—the fastest growing cancer in the U.S. based on the number of new cases.
Treating Barrett’s Esophagus
To prevent cancer in patients with Barrett’s, CentraState Medical Center is now offering an advanced, nonsurgical procedure called BarrxTM radiofrequency ablation. Radiofrequency ablation uses heat energy to destroy (ablate) diseased Barrett’s tissue in the superficial lining of the esophagus. The treatment has been shown to be more than 90 percent effective in removing precancerous tissue from the esophagus.
This ablation is an outpatient procedure done while you are under sedation. An endoscope is inserted into the esophagus, allowing your doctor to view and measure the abnormal tissue that needs to be treated. The ablation device is then inserted to precisely deliver heat energy to only the diseased tissue. The tissue is destroyed and healthy tissue eventually grows back as it heals.
The procedure takes approximately 20 minutes, and you will go home the same day. Some people will experience some pain or difficulty swallowing for a few days, but can otherwise return to normal activities the day after the procedure.
The ablation procedure is repeated every three months until the lining of the esophagus returns to normal. Most patients require three or four treatments. Additional follow-up endoscopies will monitor whether any Barrett’s tissue has returned.
I recently treated a man in his 40s who had a small, early stage esophageal cancer within a nodule in his Barrett’s esophagus. It was removed during an upper endoscopy—a procedure in which we use a thin, flexible endoscope to view the esophagus. After the superficial nodule was removed, radiofrequency ablation was able to treat the rest of the Barrett’s esophagus and heal the other areas of dysplasia.
One year since his first treatment, his follow-up exams have shown no signs of additional dysplasia, cancer or further Barrett’s esophagus.
When to See a Doctor
Many people experience occasional heartburn, especially after particularly heavy or spicy meals. If you’re having symptoms multiple times a week, you should see a doctor to determine whether GERD may be the problem.
If you are diagnosed with GERD, there are many effective treatment options available, including medications that can reduce your symptoms and help prevent the development of Barrett’s esophagus.
Award-Winning Endoscopy Care
Radiofrequency ablation is offered in collaboration with CentraState Medical Center’s endoscopy team, which was recently named an EndoNurse All-Star Team by EndoNurse magazine, a nationally acclaimed publication for endoscopy. For more information about CentraState’s services, call 866-CENTRA7 (866-236-8727).
 Dr. Amy Tilara is a board-certified gastroenterologist at Advanced Gastroenterology Associates and on staff at CentraState Medical Center. She can be reached by calling 866-CENTRA7.
Dr. Amy Tilara is a board-certified gastroenterologist at Advanced Gastroenterology Associates and on staff at CentraState Medical Center. She can be reached by calling 866-CENTRA7.





